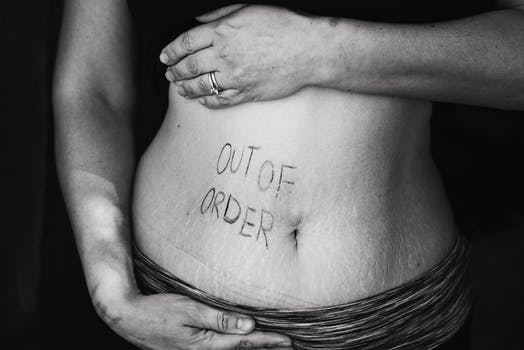
What is Irritable Bowel Syndrome (IBS)?
IBS is marked by abdominal pain, changes in bowel habits, diarrhea, constipation, abdominal distension, and other symptoms that last for three months or longer. Symptoms of IBS vary for each person and can include:
- Abdominal gas and bloating
- Alternating diarrhea and constipation
- Mucus in the stool
- Nausea after eating
- Rectal bleeding
- Abdominal pain that progresses or occurs at night
- Weight loss not explained by dieting or other health concerns
IBS can often get more complex when associated with other conditions.
These may include:
Abdominal Migraines
This is a term often given to kids who have periodic abdominal cramping and pain, vomiting, nausea. It’s a rather fancy way to say your stomach isn’t happy. In my experience as a functional medicine doctor in Singapore, this is simply a form of IBS and is therefore very treatable.
Anemia
When there is an ongoing digestive and absorption problem, anemia is very common. Anemia, a condition characterized by a lack of healthy red blood cells, can sometimes be associated with Irritable Bowel Syndrome (IBS). In individuals with IBS, particularly those with IBS-D (diarrhea-predominant IBS) or IBS-M (mixed-type IBS), chronic gastrointestinal symptoms can lead to poor nutrient absorption. This malabsorption, especially of iron and vitamin B12, can result in anemia. Additionally, chronic intestinal bleeding, though less common in IBS, can also contribute to anemia in these patients.
Celiac Disease
When symptoms do not get better on a gluten free diet, IBS may be underlying and need to be investigated. A thorough medical evaluation, including diagnostic tests and assessments led by a naturopathic doctor, is essential to differentiate between gluten intolerance and IBS. Identifying IBS is crucial as it requires a different management approach, often involving dietary changes, stress management, and sometimes medication.
Colitis and Eosinophilic Esophagitis
Colitis and Eosinophilic Esophagitis (EoE) are gastrointestinal conditions that, while distinct from Irritable Bowel Syndrome (IBS), share some overlapping symptoms and can coexist with or be confused for IBS. Colitis, an inflammation of the colon, often presents with symptoms like abdominal pain and diarrhea, similar to IBS. However, colitis is typically more associated with inflammatory changes in the colon, unlike IBS, which doesn’t cause inflammation or visible abnormalities in the gut. Eosinophilic Esophagitis, characterized by a high number of eosinophils in the esophagus, can cause swallowing difficulties and chest pain, differing from IBS. However, EoE can also present with abdominal pain and discomfort, mirroring IBS symptoms. Patients with unexplained gastrointestinal symptoms often require careful evaluation to differentiate between these conditions, as their treatments vary significantly.
Crohn’s Disease
An inflammatory condition of the intestines that can overlap with IBS symptoms. It can be associated with bacterial overgrowth, food reactions or intolerances, candida overgrowth etc.
IBS symptoms may not be the same for everyone and can change periodically. Most of the symptoms also overlap with other diseases like Gallstones, Appendicitis or cancers. When screening tests are negative for these, patients are often left with a prescription of antidepressants or motility agents for life time.
Regardless of your specific symptoms, call an expert gastro doctor in Singapore for help identifying the root cause of your discomfort. Gut health, digestive issues, anemia and more are complex issues, and they may require guidance from a trained medical professional.
What Can Trigger IBS?
Most IBS sufferers have multiple causes triggering the symptoms.
Small Intestinal Bacterial Overgrowth (SIBO)
Small intestinal bacterial overgrowth, another complex condition, happens when there is excess growth of good bacteria in the small intestine.
Food Allergies and Sensitivities
Food allergies, food sensitivities, food reactions and primary intolerances: All of these have different mechanisms and cause various symptoms. It is necessary to decipher food intolerances from other food reactions and sensitivities that promote irritation and inflammation of the intestinal lining.
Hormones Can Lead To IBS
Changes in hormones, particularly for women, can cause a cascade of changes in the body, including digestion. Menstruation is associated with exacerbation of IBS symptoms in the majority of women. Women are more likely to have IBS-C. Women with IBS are three times more likely to receive a hysterectomy than women without IBS – but hysterectomy or tubal ligation appear to have little effect on IBS severity. If you are suffering from severe symptoms during menstruation, or would like guidance through menopause, please call an experienced hormone doctor in Singapore.
Post-Infectious IBS:
Post-infectious Irritable Bowel Syndrome (PI-IBS) is a subtype of IBS that develops after an acute gastrointestinal infection, such as bacterial gastroenteritis. This condition emerges when symptoms of IBS – like abdominal pain, bloating, and changes in bowel habits – persist long after the initial infection has resolved. The exact mechanism behind PI-IBS is not fully understood, but it’s believed to involve changes in gut flora, immune system activation, and increased gut sensitivity. PI-IBS highlights the complex interaction between the gut’s immune system and its nervous system. Diagnosis typically follows a documented episode of gastrointestinal infection, and treatment strategies focus on managing IBS symptoms and supporting overall gut health.
Motility disorders: Cause constipation or diarrhea arising due to various factors from stress and emotions to chemical imbalances.
Gut Brain Axis Dysregulation
Gut-Brain Axis Dysregulation refers to the impaired communication between the gut and the brain, a critical interaction affecting both mental and gastrointestinal health. This dysregulation can lead to various disorders, including anxiety, depression, and Irritable Bowel Syndrome (IBS). It involves disruptions in the complex pathways connecting the enteric nervous system in the gut to the central nervous system. Factors like stress, diet, and gut microbiota imbalances can contribute to this dysregulation.
Exocrine Pancreatic and Stomach Acid Insufficiency
Exocrine Pancreatic Insufficiency (EPI) and Stomach Acid Insufficiency are conditions affecting digestive processes. EPI occurs when the pancreas fails to produce enough digestive enzymes, leading to malabsorption and nutrient deficiencies. Symptoms include diarrhea, weight loss, and abdominal pain. Stomach Acid Insufficiency, on the other hand, involves inadequate production of gastric acid, essential for food digestion and nutrient absorption. This can result in bloating, indigestion, and an increased risk of gastrointestinal infections.
How a Naturopathic Doctor Looks For The Cause of IBS
My approach to IBS differs from conventional treatments. Once a diagnosis of the cause is established through required testing and physical exams, I look for contributing factors that are obstacles to cure before initiating any treatments. More recently, I am also screening for sleep disorders and Histamine imbalances that contribute to the Gut and Hypothalamus pituitary adrenal axis imbalance.
Identifying these unique imbalances in different systems for each individual–neurological endocrine, immune and gastrointestinal–helps provide a comprehensive and targeted treatment plan for long term management of IBS. I do not simply prescribe medication and send you on your way.
How To Naturally Treat IBS
Treatments vary depending on the cause and triggers in each individual. After stimulating the vital force of the body and removing obstacles to cure, I often use a stepped approach for long term positive outcomes in IBS through Herbs, homeopathy and targeted supplements and Psycho/behavioral interventions that work towards,
- Stabilizing adrenal and immune function if there is HPA dysregulation.
- Modifying dysbiotic lifestyle factors (factors in one’s lifestyle that promote microbial imbalances).
- Implementing a sustainable microbiome diet.
- Stabilizing the microbial flora.
- Improve motility of the intestines.
- Replenish nutrients that promote digestive and immune factors.
- Restore gut barrier/ intestinal permeability.
Irritable bowel does not have to be a life sentence. As you can see it’s a complex puzzle with a variety of potential interrelated causes. The point is, there is definitely a cause. If you have a digestive problem and no one has been able to help you with it, don’t give up. We have treated a considerable number of patients at the clinic successfully with this comprehensive approach.
Reference Material:
1.Ghoshal UC, Srivastava D. Irritable bowel syndrome and small intestinal bacterial overgrowth: meaningful association or unnecessary hype. World J Gastroenterol. 2014;20(10):2482-2491
Thompson JR. Is irritable bowel syndrome an infectious disease. World J Gastroenterol. 2016;22(4):1331-1334
Lee YJ, Park KS. Irritable bowel syndrome: emerging paradigm in pathophysiology. World J Gastroenterol. 2014;20(10):2456-2469.
Zhang L, Song J, Hou X. Mast Cells and Irritable Bowel Syndrome: From the Bench to the Bedside. J Neurogastroenterol Motil. 2016;22(2):181-192
Wilkins T, Pepitone C, Alex B, Schade RR. Diagnosis and management of IBS in adults. Am Fam Physician. 2012;86(5):419-426
Morito Y, Aimi M, Ishimura N, et al. Association between sleep disturbances and abdominal symptoms. Intern Med. 2014;53(19):2179-2183.
Akahashi T. Interdigestive migrating motor complex -its mechanism and clinical importance. J Smooth Muscle Res. 2013;4999-111.
Hayes PA, Fraher MH, Quigley EM. Irritable bowel syndrome: the role of food in pathogenesis and management. Gastroenterol Hepatol (N Y). 2014;10(3):164-174



Hello Dr Kamat,
Have you any experience treating patients with autoimmune hepatitis?
Hi Marilyn,
Thank you for getting in touch.
Autoimmune hepatitis often has infectious history especially viruses. Exploring the root cause is necessary.
Certain herbs that are immune modulating and protects liver from damage could be beneficial.
Diet plays a crucial role in these cases, a carefully chosen ellimination diet could help reduce inflammation. Should you wish to consult or explore more options, please give us a call. Best, Dr K
Best,